
Outbreaks and emergencies can have a significant impact on people’s mental health. However, there is limited evidence to inform the inclusion of mental health and psychosocial support (MHPSS) in outbreak planning, or to understand how feasible implementing MHPSS interventions during outbreaks is.
The MHPSS Minimum Service Package outlines a set of activities that are considered to be of the highest priority in meeting the immediate critical needs of those affected by emergencies. The MSP is based on the Inter-Agency Standing Committee MHPSS guidelines, incorporating available evidence and expert consensus over recent years. It is relevant for all emergencies, but has specific considerations for public health emergencies and outbreaks.
|
MHPSS Minimum Service Package - explained
|
Working closely with researchers based at Makerere University, the Ministry of Health in Uganda and Africa CDC, this study aims to use the MSP to develop, implement and evaluate a suite of tailored MHPSS interventions that could be used to support outbreak preparedness and response in Uganda.
Firstly, the project team used the MSP to create a tailored, context-specific set of MHPSS interventions for outbreak responses in Uganda. The team then developed a plan to deliver the recommended interventions, including community engagement and capacity strengthening activities.
Research project activities
November 2024Workshop: Orienting frontline workers and community leaders in basic psychosocial support skills 23 participants were trained about the basics of mental health and psychosocial support. This included members of the Bundibugyo community such as bus drivers, sex workers and businesspeople – ensuring the training was relevant to the every-day lives of people living in the district. Topics included how to look after their own mental health and how to talk to others in their community about mental health within the context of the active mpox outbreak. The workshop also generated specific key messages about the importance of mental health support during the mpox outbreak to be used in the Bundibugyo community to raise awareness and encourage people to reach out for support. Photo credits: MoH Uganda |
|
December 2024Workshop: Embedding mental health care as part of general health services This training focused on increasing the knowledge of non-mental health specialist health care workers of best practice when interacting with patients, specifically in the context of the ongoing mpox outbreak. 30 participants were trained from a range of areas, from hospitals and small health clinics to healthcare workers in the prison service – ensuring the training could impact the most vulnerable in society who are often overlooked. Teaching was based on the WHO developed mhGAP toolkit which is used to train healthcare works in mental health skills. The participants learnt how to recognise, treat and reduce stigma towards individuals facing complex mental health problems including depression, acute stress, post-traumatic stress disorder and other conditions. Photo credits: MoH Uganda |
|
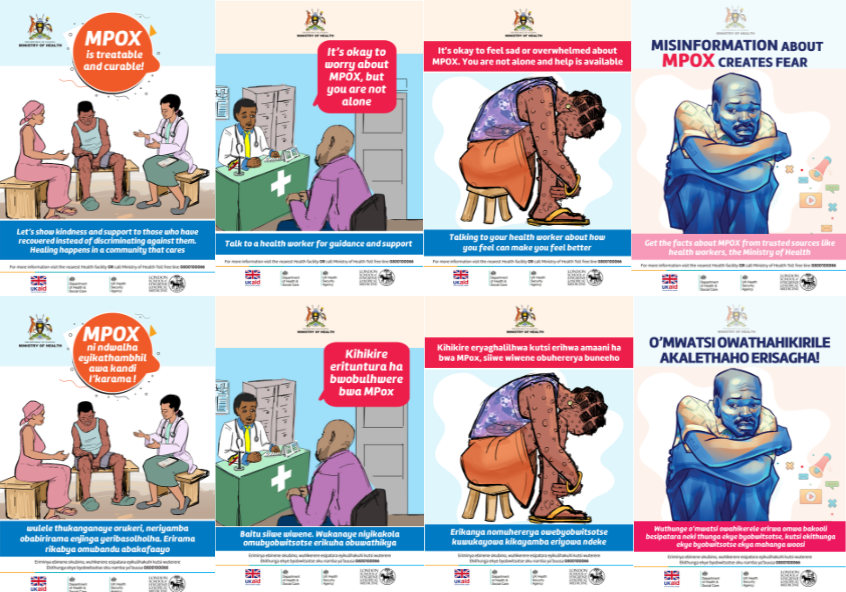
March 2025Raising community awareness: Sharing resources to promote mental health and psychosocial wellbeing in Bundibugyo Following the success and learnings from the previous workshops, the study team created awareness posters, radio messages and talk show recordings using community-specific key messages. These resources were distributed to the local community to raise awareness of mental health services in the district and encourage their uptake during the mpox outbreak. Image credit: Ministry of Health Uganda
|
 |
March 2025Testing MHPSS readiness: Community tabletop exercise The Uganda Ministry of Health, with design and delivery support from the UK-PHRST, organised a tabletop exercise to assess MHPSS interventions in Uganda by bringing together stakeholders from the Ministry of Health and district health teams from Bundibugyo and Kasese districts. The team used a tabletop exercise to simulate outbreak scenarios that might happen in real life, allowing stakeholders to work through what their response might be. The tabletop exercise in Uganda both assessed the MHPSS preparedness and response status at the national and district levels and acted as a learning exercise by highlighting gaps in current response capacity. The exercise brought out practical lessons and recommendations to improve response in future disease outbreaks. Photo credits: MoH Uganda |
|
The MHPSS interventions will be evaluated to understand whether they are well accepted and taken up, are feasible to implement and are appropriate to the response. In parallel, the team is working to understand the experiences of frontline healthcare workers in outbreak response, to develop wellbeing plans to mitigate the impact of outbreaks on their mental health.
As a result of the research project, in September 2025, the MHPSS team also supported a workshop to help strengthen outbreak preparedness and mental health response capacities in Uganda. Co-organised with Uganda’s Ministry of Health, Makarere University and TPO Uganda, the workshop brought together participants from the Ugandan Ministry of Health and outbreak response co-ordinators from the Ugandan Incident Management System.
|
Julian Eaton, Mental Health and Psychosocial Support Lead, UK-PHRST said: “Outbreaks and emergencies can have a significant impact on people’s mental health. The mental health and psychosocial support Minimum Service Package is a very practical, evidence-based resource for organisations involved in humanitarian emergency response to follow, and is very appropriate for outbreaks of infectious disease. In collaboration with mental health experts at Makerere University and Africa CDC, we are using the Minimum Service Package to develop a tailored set of interventions that can be successfully and sustainably delivered by outbreak responders in Uganda. We hope this research will improve the mental health and wellbeing of communities affected by outbreaks across the country, and help us better understand how we can build community resilience.” |






